By: Michael Eid
Read more guides on Endodontics by Michael Eid:
Endo diagnosis isn’t about memorizing tests. It’s about pattern recognition. Here’s how to get it right without overthinking it.
1. Listen Before You Touch the Tooth
The story usually gives the answer.
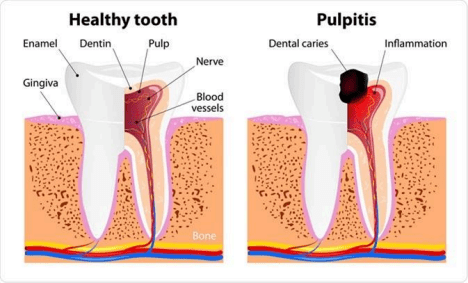
- Cold lingers → pulpitis
- Pain wakes them up → pulpitis
- Biting pain → apical involvement
🦷 Tip: If the history doesn’t fit the diagnosis, you’re probably wrong.
2. Cold Test Is King
Cold tells you more than EPT.
- Sharp, quick, gone → normal/reversible
- Lingers >10–15 sec → irreversible pulpitis
- No response → necrosis (confirm with something else)
🦷 Tip: Always compare to a control tooth.
3. Heat Means Trouble
Heat pain usually = advanced pulpitis or necrosis with gases.
🦷 Tip: If cold doesn’t hurt but heat does, think necrotic pulp with apical disease.
4. Percussion = PDL Status
Tender to bite or tap = apical inflammation.
🦷 Tip: Percussion doesn’t diagnose the pulp — it diagnoses the apex.
5. Palpation Confirms Spread
Tender mucosa or vestibule = inflammation has escaped the tooth.
🦷 Tip: Swelling + percussion pain = endo until proven otherwise.
6. Don’t Overtrust the Radiograph
Early endo disease often looks normal.
- No PA lesion ≠ healthy tooth
- Lesions lag behind symptoms
🦷 Tip: Symptoms > X-ray.
7. Isolate the Tooth Properly
Use cotton rolls, dry field, one tooth at a time. Tip: If multiple teeth hurt to cold, you didn’t isolate well.
8. Cracked Tooth ≠ Endo (Until Proven)
Sharp pain on release = crack until proven otherwise.
🦷 Tip: Endo hurts going down. Cracks hurt coming up.
9. Localize Before You Treat
If you can’t point to one tooth, stop.
- Re-test
- Re-question
- Re-evaluate
🦷 Tip: Never do endo on a “suspected” tooth.
10. When in Doubt, Step Back
Endo diagnosis rewards patience.
🦷 Tip: A delayed diagnosis is better than the wrong tooth.

